What is Trigger Finger Surgery (Trigger Finger Release)?
May 2nd, 2016 | 4 min. read


If your finger or thumb gets locked in a bent position or straightens with a loud POP!, you may have trigger finger or trigger thumb. This condition isn't dangerous, but it can bring discomfort, and it may get in the way of your everyday activities.
Many people with trigger finger find it difficult to perform repetitive tasks that involve grasping or holding things like tools, controls, steering wheels, a computer mouse, or even a coffee cup.
They may also experience pain, tenderness, or stiffness in any of their digits (most commonly in the index finger, middle finger, or thumb).
If you're suffering from trigger finger or trigger thumb, you may want to make an appointment to see an orthopedic doctor. Read on to learn more about this condition and how you can fix it.
What Is Trigger Finger (or trigger thumb)?
Trigger finger or trigger thumb is a condition in which a finger catches or locks when bent, and may snap or pop loudly when pulled and released — much like a gun's trigger.
The medical term for trigger finger is stenosing tenosynovitis. Some refer to it as "snapping thumb syndrome."
Why trigger finger occurs
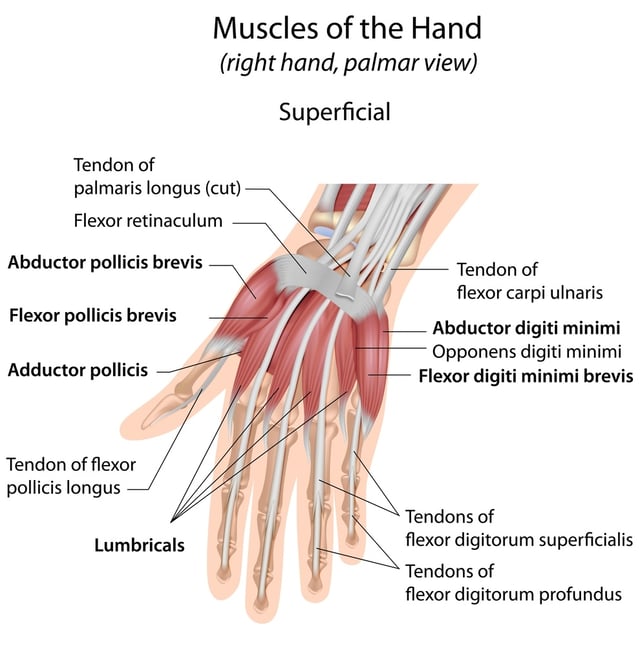
The medical cause is inflammation of the flexor tendon, which controls the finger's ability to bend and straighten.
This tendon passes through a narrow tunnel called the tendon sheath.
When the flexor tendon is healthy, it glides easily through this sheath. If the tendon is irritated, inflamed, or scarred, however, it can thicken or form nodules (bumps), which makes the passage through the tunnel difficult.
Trigger finger occurs when the enlarged or irritated tendon becomes stuck in the tendon sheath, causing the finger or thumb to remain in a bent position.
Stenosing tenosynovitis varies in its severity. Some fingers may suddenly pop out when pulled straight. Others may remain stuck in a bent position.
Risk factors and causes
- Trigger finger is more common in women.
- It is more common in people with diabetes or rheumatoid arthritis.
- It is most often seen in people ages 40 to 60, though bilateral (affecting both thumbs) trigger thumb can be congenital; some children are born with it and can have it corrected surgically when they get older.
- Repetitive strain is often the cause of trigger finger in adults. Performing the same movements over and over, particularly gripping actions, can lead to inflammation that may cause fingers to trigger.
Symptoms
Trigger finger more commonly affects the thumb, the middle finger, or the ring finger. More than one finger can experience triggering at one time, and symptoms can occasionally be bilateral (involving both hands).
Symptoms can be mild to severe and may progress over time. They can include:
- Finger stiffness, especially in the morning
- Finger catching or locking in a bent position, which suddenly pops straight
- Finger locking in a bent position, which you are unable to straighten
- A popping or clicking sensation when you move your finger
- Tenderness, swelling, or a bump (nodule) in your palm at the base of the affected finger
- Pain or discomfort
Getting diagnosed
If you're experiencing any of the above, your doctor can perform an exam.
To diagnose trigger finger, your doctor may ask you questions about your symptoms, including how long you've been experiencing them and if any hobbies, sports, or other activities may have contributed to your hand injury.
Your doctor will examine your hand to search for nodes or lumps that may be attached to the tendon. You'll also be asked to open and close your hand to check for locking.
No X-rays are usually required to diagnose trigger finger. Depending on the severity of your injury, your doctor may refer you to an orthopedist to discuss injections or surgical treatment options.
Non-surgical treatments for trigger finger
Conservative, non-invasive approaches may help ease your symptoms. These include:
- Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen (Advil, Motrin IB) or naproxen (Aleve) for pain. These will not help restore range of motion, but they may reduce your discomfort. The same is true for other home remedies or natural remedies.
- Rest. For 3-4 weeks, avoid activities that require repetitive or prolonged gripping or grasping (such as using power tools, operating heavy machinery, biking, or golfing).
- Ice or heat. You may get temporary relief from stiffness or pain by icing your palm or soaking your hand in warm water.
- A splint or hand brace. Wearing a splint or brace when you sleep may keep your fingers straight, allowing your tendon the opportunity to rest. A splint can prevent you from sleeping with your hand in a fist, which can result in stiffness and loss of mobility in the hand when you wake up. Be sure to talk to a doctor before splinting.
- Stretching. Gentle exercises, under the direction of a doctor, may help maintain mobility in your finger.
- Cortisone (steroid) injections. This is the most common treatment for trigger finger or thumb. Injections into the tendon sheath or near the tendon are effective in up to 90 percent of patients (the results are less effective in patients with underlying conditions like diabetes or rheumatoid arthritis). The goal is to reduce inflammation, allowing the tendon to glide freely. Two to three injections may be needed. If you still have trouble after two to three injections, surgery may be recommended.
trigger release surgery
Trigger finger release surgery is often the most successful way to restore full motion to a trigger finger or trigger thumb. Two main kinds of hand surgery are performed to release the tendon:
1. Percutaneous release
In this trigger finger surgery, your doctor will numb your palm and insert a needle into the tissue around your tendon. Using ultrasound to guide her, she'll move the needle and your finger to help break apart the constriction that's blocking the smooth motion of the tendon.
This procedure is usually done in the doctor's office or procedure room.
2. Open trigger finger release (preferred)  This trigger finger surgery is also known as trigger thumb release, trigger finger repair, or trigger finger pulley release.
This trigger finger surgery is also known as trigger thumb release, trigger finger repair, or trigger finger pulley release.
Because this procedure allows doctors to see and access the tendons and sheath without the risk of harming surrounding nerves, many surgeons prefer open release over percutaneous release.
Open trigger finger release surgery is performed by an orthopedic surgeon on an outpatient basis.
After administering a local anesthetic to numb your hand, your surgeon will use a scalpel or needle tip to make a small incision in the palm. This allows access to the tendon tunnel sheath.
The surgeon will then cut the tendon tunnel sheath to widen its opening, allowing the tendon to slide through. You'll receive stitches to close the wound.
When the tendon sheath heals, it will be looser, allowing the tendon more room to move.
POST-SURGICAL recovery
After trigger finger surgery, most people are able to move their fingers or thumbs immediately. You may be able to write or use a computer immediately, and most people return to driving within three to five days.
For sports, you may need to wait two to three weeks before your grip returns to its previous strength.
Full recovery takes about six weeks; however, you may experience palm soreness, swelling, or stiffness which can take up to six months to resolve.
For best results, be sure to follow your surgeon's recommendations for pain relief, physical therapy or sports medicine, and exercise.
when to consult an ORTHOPEDIC SURGEON
If your finger or thumb catches, an assessment may be a good idea. Give Coastal Orthopedics located in Corpus Christi, TX a call. Our orthopedic specialists can assess your condition and discuss whether trigger finger or trigger thumb release surgery may be an option for you. Telephone: 361.994.1166.
Article written by: Rob Williams, MD
Dr. Williams has been practicing orthopedic surgery in Corpus Christi since 1998. After graduating from Texas Tech hereceived his medical degree from the University of Texas at San Antonio. At the prestigious Campbell Clinic located at the University of Tennessee, Dr. Williams completed not only an Orthopedic Surgery Residency, but an additional year of Fellowship Training in Spine Surgery. Dr. Williams is dedicated to creating an excellent patient experience in the office or in the surgery suite.
Topics:


