Achilles Tendon Rupture: Treatment, Therapies, and Recovery
June 13th, 2016 | 5 min. read

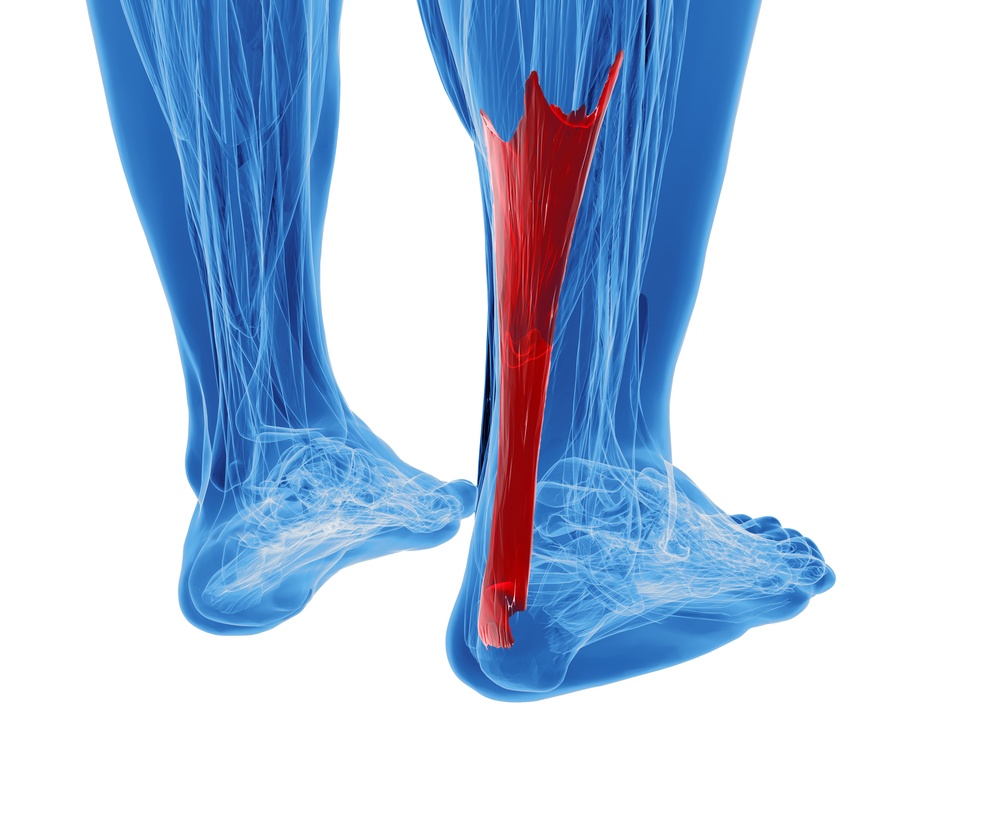
The Achilles tendon is the thickest tendon in the body, running alongside the back of the lower leg and ankle. It connects the heel bone (calcaneus) to the muscles at the back of the calf and controls the raising and lowering of the heel.
The Achilles tendon is one of the most frequently injured tendons, especially among athletes. A sore Achilles can affect your walking, running, and sports performance. A ruptured Achilles tendon, however, is far more serious and may require surgery.
How do you know if you have an Achilles tendon rupture — and what are your options for treating it?
What is an achilles tendon rupture?
An Achilles tendon rupture is a tear in the tendon, usually occurring during a sudden upward flexing of the ankle (called dorsiflexion) or pointing of the toe (called plantarflexion).
The motions may be the result of activity, or they could come from a sudden and unexpected over-flexing of the foot beyond the normal range of motion (for example, upon impact in an accident or when rolling an ankle when walking on an uneven surface).
An Achilles tendon tear can be a partial tear (meaning your tendon is still attached to the calf muscle) or a full rupture (the tendon has pulled apart completely; your heel no longer connected to your calf muscle by the Achilles tendon).
If you tear your Achilles, you may still be able to walk with a limp. You may even be able to raise your heel off the ground, with some discomfort or pain.
If you rupture your Achilles, however, you will no longer be able to stand on tiptoe or lift your heel off the ground because the tendon controlling that motion has been severed. Pointing your toe may also be difficult. (More symptoms of an Achilles tendon rupture are listed below.)
Athletes (and non-athletes) sometimes rupture their Achilles tendons while:
- jumping
- accelerating explosively
- pushing off
- twisting the foot/ankle
Any sudden force put on the tendon can lead to a partial tear or complete tear.
Other risk factors for Achilles tendon rupture include:
-
taking fluoroquinolone antibiotics over a long period (for example, ciprofloxacin); these medications are known to increase the risk of having weakened or ruptured tendons
-
suddenly increasing physical activity after long periods of inactivity (e.g., being a "weekend warrior"); working unconditioned muscles and tendons can lead to injury
-
having tight muscles and tendons; tightness and lack of flexibility can inhibit your range of motion, making sudden movements more likely to result in tears
-
pre-existing Achilles tendinitis (acute tendon injury with inflammation)
- pre-existing Achilles tendinosis or tendinopathy (chronic tendon injuries, with or without inflammation)
An orthopedic specialist will be able to examine you and take a full medical history to assess your condition and your risk.
Who ruptures their Achilles? Individuals with increased risk include:

- men — about five times as likely as women to sustain Achilles ruptures
- anyone starting a new or intense physical activity without gradually conditioning first
- athletes playing sports requiring explosive start-and-stop movements or jumping (basketball, diving, gymnastics, tennis)
- hikers and walkers (especially when walking on uneven surfaces)
- runners
- obese or overweight people
- older individuals (especially those with arthritis)
- people with prior histories of Achilles tendon tears or tendon injections (for example, corticosteroids)
- people with a history of taking fluoroqinolone antibiotics, which has been shown to cause to tendon weakness and rupture in some individuals
You're also more likely to re-rupture your Achilles tendon if you ruptured it in the past but treated it conservatively at the time (without surgery).
Take a look at your footwear, as well; if your shoes are old and worn out or have too little support for your heel and arches, you may be more at risk for injury.
Symptoms of an Achilles tendon rupture
Some people who rupture their Achilles notice symptoms before the injury occurs — for example, heel pain or soreness or a swollen ankle, indicating inflammation, a small tear, or tendinitis.
Others won't have any signs or symptoms and may experience the rupture as a sudden, "out of nowhere" injury.

Either way, if you have ruptured your Achilles tendon, you'll experience some or all of the following:
- a snap at the back of the heel
- pain in the back of the ankle
- immediate weakness in the affected foot/ankle, limping, and difficulty walking (flat-footed walking only)
- Inability to climb stairs or stand on your toes (because you can no longer raise your ankle)
- bruising around the ankle
- swelling of the ankle
If you think you've sustained an Achilles tendon rupture, see a doctor immediately. If you wait to get treatment, you may end up prolonging your recovery.
achilles tendon rupture: therapies & surgery
If you've torn your Achilles tendon, treatment may include non-surgical or surgical repair. A diagnosis and exam by an orthopedic doctor is your first step in determining the best way to treat and rehab your Achilles rupture.
During the exam, your doctor may look for a soft tissue depression in your ankle or heel, which can indicate a tear in the tendon. He or she may also order an ultrasound or MRI test to confirm whether your tear is partial or a full rupture.
Non-surgical treatment for Achilles tendon rupture
Immediately after any Achilles tendon injury, before you can get to a doctor, you can treat your injury with RICE (rest, ice, compression, elevation) and over-the-counter pain relievers with anti-inflammatory properties (such as ibuprofen, naproxen, or acetaminophen).
If you and your orthopedist choose a conservative, non-surgical treatment for your rupture, treatment may require casting your foot with your toe pointed, then re-casting periodically to gradually decrease flexion as you heal.
Non-surgical casting is sometimes recommended for patients who are not healthy enough to undergo surgery. If you have an active infection, for example, or a pre-existing condition like diabetes, your doctor may recommend a non-surgical approach.
However, if you are healthy, active, and want to get back to your normal activities faster, your doctor may recommend surgery, largely because the incidences of re-rupture are far lower after surgical repair.
Up to 30% of patients who treat their ruptures non-operatively later re-rupture their Achilles, vs. a 3–5% re-rupture rate among those who choose surgical repair.
Achilles tendon rupture surgery and repair
Surgical repair of an Achilles tendon rupture is usually performed on an outpatient basis at a surgical center, and most patients can return home the same day.
Two types of Achilles repair procedures are available:
- Open surgery. In this procedure, the nerve block in the affected leg is numbed and the patient is put under general anesthesia. The surgeon will make an incision to the back of the leg, just above the heel. After locating the ends of the ruptured tendon, he or she will suture them together. This surgery takes between 30 minutes to an hour or more.
- PARS (Percutaneous Achilles Repair System) surgery. This relatively new, specialized technique allows a surgeon to repair a ruptured tendon using a much smaller incision (about two centimeters in size). A PARS device is inserted to hold the tendon in place. The device creates small holes in the skin around the site of injury. The surgeon can then insert needles through these holes to suture the ends of the torn Achilles together. This procedure is for new injuries only.
Achilles TENDON RUPTURE: recovery

After either form of Achilles tendon rupture repair, expect to wear a cast and/or walking boot for a total of 6 to 12 weeks.
Immediately after surgery, your foot will be immobilized with your toe pointed. In subsequent office visits, the doctor will gradually adjust the position of your foot to a more neutral position as the tendon heals.
During the first six weeks or so of your healing, your doctor will instruct you not to walk on the recovering leg — it cannot bear weight. During this recovery period, you may keep weight off your foot using:
- crutches
- knee scooter/knee walker
- wheelchair
Once you can bear weight again, you'll begin physical therapy. Your therapist may use a combination of techniques, including gentle stretching, strengthening, aquatic therapy, ultrasound, and massage to help promote healing and to get you back to walking with a full (or close to full) range of motion.
Recovery time varies, depending on many factors. If you're in good general health and are committed to following your doctor's instructions and practicing your physical therapy exercises regularly, you may be able to fully return to former activities in four to six months.
However, athletes should note that even with surgery and a full course of physical therapy, the Achilles tendon may never be as strong or as flexible as it was prior to injury.
An orthopedic specialist can help you discuss your options and create a plan for treating your Achilles tendon rupture or Achilles tendinitis. Give Coastal Orthopedics located in Corpus Christi, TX a call and ask for a consultation. Telephone: 361.994.1166.
Article written by: Rob Williams, MD
Dr. Williams has been practicing orthopedic surgery in Corpus Christi since 1998. After graduating from Texas Tech hereceived his medical degree from the University of Texas at San Antonio. At the prestigious Campbell Clinic located at the University of Tennessee, Dr. Williams completed not only an Orthopedic Surgery Residency, but an additional year of Fellowship Training in Spine Surgery. Dr. Williams is dedicated to creating an excellent patient experience in the office or in the surgery suite.
Topics:

