WHAT IS DEGENERATIVE DISC DISEASE? (SIGNS AND SYMPTOMS)
June 26th, 2017 | 5 min. read
If you’re approaching 40, or older, and you find yourself dealing with either acute or chronic lower back pain or neck pain, you may have degenerative disc disease, or DDD.
Degenerative disc disease refers to the natural, age-related breakdown of the intervertebral discs of the spine—the fluid-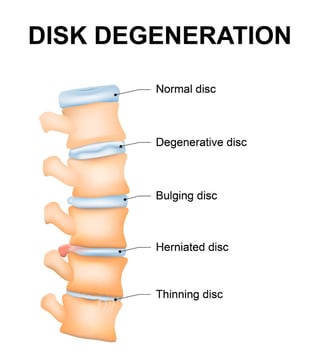 filled cartilage “spacers” that provide cushioning between each of your back bones. Think of the discs as shock absorbers; they’re designed to provide flexibility and to reduce stress on your spine.
filled cartilage “spacers” that provide cushioning between each of your back bones. Think of the discs as shock absorbers; they’re designed to provide flexibility and to reduce stress on your spine.
Though we refer to DDD as a disease, in actuality it’s a process—a mostly natural byproduct of age-related wear and tear. (However, some people, such as athletes or people involved in accidents, may experience DDD sooner than expected due to trauma to the spine.)
As we get older, the everyday forces that compress, twist, and otherwise act upon our spines eventually cause the rubbery discs to break down, shrink, and sometimes, to collapse completely. Disc collapse like this can put pressure on nerve roots in or near the spine.
It can also lead to bone-on-bone friction, which can lead to other spinal conditions like osteoarthritis, bone spurs (bony overgrowths—themselves harmless, but they can cause other problems to nearby tissue), sciatica (a pinched or inflamed nerve), and spinal stenosis (a narrowing of the spinal canal’s available space).
Disc degeneration may cause pain and other symptoms, and it can create a domino effect of complications in and near the spine—but unlike many diseases, it’s not something you are likely to “catch” or develop due to environment or genetics.
By and large, degenerative disc disease is something that just happens—to most of us, eventually. According to The Arthritis Foundation, nearly everyone over the age of 60 has some form of degeneration of the spine.
However, in some cases, lifestyle changes like quitting smoking, losing weight, and gently exercising may help to slow it down and minimize the damage it causes.
Intervertebral Discs and How They Degenerate
The normal human spine has 23 discs. Most (12) are in the middle-back (thoracic region). Six are in the neck (cervical region) and five are in the lower back (lumbar region).
Each intervertebral disc is made of two major components:
- The annulus, a fibrous outer ring which provides stability and shape to the disc; the annulus is made of multiple layers of collagen fiber and is strong enough to withstand high compressive forces.
- The nucleus pulposus, a gel-like center which provides cushioning to the spine, in part by distributing pressure evenly across its surface. (Similar to the principle of lying down flat when you’re on thin ice; spreading out a weight or pressure reduces its impact on any single point.) A healthy nucleus pulposus can take in additional water and swell, allowing it to function normally.
As we age, the nucleus pulposus gradually loses its ability to hold water. This gel-like center, or matrix, also contains a concentration of proteins that allow it to absorb shock; these proteins become less dense as we get older.
The outside of the disc, the annulus, degrades too. It’s collagen-based; like most collagen and cartilage in our bodies, it becomes weaker, dryer, and more brittle over time, which makes it more vulnerable to tears and cracks. (Sometimes resulting in the nucleus pulposus pressing outside of its shell—what we call a herniated or bulging disc.)
Who Has Disc Degeneration?
- Adults under 40. Researchers estimate that about 1 of every 4 adults under the age of 40 is living with some degree of degeneration. (Not everyone will feel symptoms like back pain at this age, however.)
- Adults over 40. About 60% of all adults over 40 are living with some degree of DDD. (Again, not everyone will have back or neck pain. . .yet.)
- Adults over age 60. Researchers reviewing MRI scans estimate that almost 100% of adults over 60 have some degree of spinal degeneration—and yes, probably some back or neck pain, too, along with loss of height or curvature of the spine (a hump).
Essentially, just about everyone will experience DDD eventually. However, no two individuals will have exactly the same symptoms or repercussions on the same timetable.
Causes of Disc Degeneration
Again, DDD isn’t really a disease, it’s a condition that involves intervertebral discs losing their integrity as they age. Over the course of a lifetime, it’s natural for our discs to become thinner, less hydrated, and less able to cushion the spine.
However, certain factors can contribute to DDD. These include:
- If you’re over 40, you’re more likely to have moderate degeneration, to the extent that you begin to notice symptoms like back pain or related issues like sciatica.
- Studies show that smoking can negatively affect the vascular system, inhibiting the body’s ability to use its blood supply to heal a torn or injured disc. Smoking may, in fact, speed up spinal degeneration. It can also create instability in ligaments, which may make the back more prone to injury.
- People who carry a lot of excess weight are more likely to show symptoms of DDD. Being obese is a force multiplier that subjects the body to more strain.
- Exercise/wear-and-tear. Excessive sports or work-related strain may contribute to tears in the outer disc wall. Lifting with your back and not your legs, for example, can cause a tear followed by a herniation. Such injuries can happen at any age, but are more likely in people over 40, who’ve already begun to experience disc degeneration.
- An acute injury or trauma to the spine (for example, from a motor vehicle accident or a fall) may force the herniation of a disc. Such an injury can can begin the process of degeneration because discs receive a low blood supply in general; an injured disc cannot easily repair itself. Also, the resulting instability and swelling from a tissue injury can also put additional pressure on the spine and surrounding nerves.
Signs & Symptoms of degenrative disc disease
Degenerative disc pain tends to happen in the neck (cervical disc degeneration) or the lower back (lumbar disc degeneration). Some people do not feel symptoms at all, while others may have severe and disabling pain.
Symptoms vary depending on where the affected disc is located and how great the damage is. A more degraded disc, for example, will mean less space between the two vertebrae. This can create more friction and more pressure, and that may in turn cause nerve impingement, inflammation, bony overgrowths, or other issues.
Common symptoms can include pain, tenderness, numbness, and weakness:
- Pain in the lower back, buttocks, thigh, or neck. This can range from a nagging soreness to severe and disabling pain that keeps you from walking comfortably, turning your head, or participating in activities. Pain may feel chronic and constant or it may flare up occasionally for a period of time.
- Pain that’s worse when you’re sitting or inactive, but which improves when you’re walking or moving around.
- Pain that occurs when you twist, bend at the waist, or lift objects.
- Pain that improves temporarily when you change your body position or lie down.
- Pain that radiates; for example, it may start in the neck and move to the arms and hands; this may indicate an affected nerve near the neck.
- Pain that is severe and which comes in bouts of a few days to a few months.
- Numbness, pins and needles, or tingling in your hands or feet; this may indicate nerve impingement or swelling.
- Weakness in the legs, which may mean you have nerve impingement or damage; foot drop is a common form of this nerve damage. Sciatica is another.
Degenerative disc disease is common and many of its symptoms are treatable with exercise, medicine, physical therapy or even surgery. However, it must be diagnosed in a doctor’s office before you begin a treatment plan.
If you would like to speak with an orthopedist about this condition, please call Coastal Orthopedics in Corpus Christi today at (361) 994-1166.
Article written by: Rob Williams, MD
Sources:
http://www.mdguidelines.com/intervertebral-disc-disorders
http://www.arthritis.org/about-arthritis/types/degenerative-disc-disease/
https://www.ncbi.nlm.nih.gov/pubmed/11339862
Dr. Williams has been practicing orthopedic surgery in Corpus Christi since 1998. After graduating from Texas Tech hereceived his medical degree from the University of Texas at San Antonio. At the prestigious Campbell Clinic located at the University of Tennessee, Dr. Williams completed not only an Orthopedic Surgery Residency, but an additional year of Fellowship Training in Spine Surgery. Dr. Williams is dedicated to creating an excellent patient experience in the office or in the surgery suite.
Topics:

