Plantar Fasciitis In runners | What is it & how can it be treated
July 17th, 2019 | 4 min. read


Planter fasciitis is a common cause of heel pain. When you first wake up in the morning and swing your feet out of bed, do your first few steps feel stiff or painful? Or does your heel hurt when you stand up after a long time sitting? If so, you may have the condition known as plantar fasciitis: an inflammation or swelling of the band of tissue along the bottom of your foot.
Although the pain from plantar fasciitis is normally worse with the first few steps and can resolve, the condition may become chronic if ignored. Not only could this cause nonstop heel and foot pain, it could adversely affect how you walk — contributing to leg, hip, and back problems.
What is the Plantar Fascia?
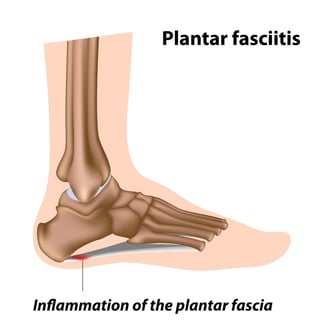
A thick, broad, flexible sheet of tissue runs all across the bottom of the foot, connecting the heel to the base of every toe. This sheet of connective tissue is the plantar fascia (plantar refers to “the bottom of the foot;” fascia are thin sheets of tissue covering most organ).
The plantar fascia behaves like a shock absorber for the arches of your feet. With every step you take, it stretches, and supports your body’s entire weight.
What is Plantar Fasciitis?
Plantar fasciitis can be thought of as an “over-use injury” to the arch of your foot.
While the plantar fascia is remarkably strong and flexible, if it is subjected to too much stress, it can tear — just like a sheet of over-stretched fabric.
Tiny tears can easily be self-repaired by the body, but repeated or large tears can cause much greater inflammation, which is what causes the pain and stiffness of plantar fasciitis.
What causes Plantar Fasciitis?
Plantar fasciitis occurs in both men and women, most often between the ages of 40 and 70. In most cases, this condition begins with mild pain in the heel, which if untreated can spread through the entire arch of the foot.
Typical causes include:
- Exercise. Engaging in physical activities that cause high stress on the feet, such long-distance running on downhill or uneven surfaces, ballet, and high-impact aerobics.
- Footwear. Wearing poorly-made shoes with soft soles or poor arch support.
- Weight. Being obese, or experiencing sudden, significant weight gain.
- Anatomy. Having flat feet, high arches, or tight calves or Achilles’ tendons.
- Occupation. Having a job that requires walking or standing for many hours at a time on hard surfaces.
- Sudden changes in activity. Taking up new or intense physical activities without slowly conditioning the body ("weekend warrior syndrome").
How do I know if I have plantar fasciitis?
This condition can occur suddenly, or develop over a long period of time. The classic symptom is a sharp, stabbing pain in your heels when you take your first steps in the morning. The pain normally subsides after a few paces.
Other typical symptoms include heel pain from any or all of the following activities:
- climbing steps
- intensive exercise — pain that comes after (e.g., aerobics, running)
- standing up after sitting for extended periods
- standing on hard surfaces for a long time
Your doctor normally can diagnose plantar fasciitis based entirely on a history and physical exam.

Indicators include:
- limited upward flexibility of the ankle
- tenderness on the sole of your foot, just in front of the heel, that gets worse when pressed
- pain when toes are flexed upwards and pressure is applied to the bottom of the foot
- reduced pain when toes are pointed downwards and pressure applied to the bottom of the foot
If your doctor believes your pain is being caused by something else, such as a pinched nerve or stress fracture, an X-ray or MRI may be taken.
Ultrasound imaging is not normally used to diagnose this condition. Bone spurs are no longer considered to be among the causes of plantar fasciitis.
How can i treat plantar fasciitis?
You may treat this condition using simple home remedies. Non-surgical remedies have a very high success rate, with such treatments lasting from nine to twenty-four months.
For immediate relief, you may try the following:
- Hold an ice pack to the bottom of your feet for five to ten minutes, at least two times a day, for a few days.
- Take over-the counter medication, such as acetaminophen, naproxen, or ibuprofen, to reduce pain and inflammation.
- Stay off your feet as much as possible for 5–7 days.
- Do gentle stretches for your Achilles and arch.
For longer-term treatment, you may:
- Insert shoe inserts or heel cups into your shoes.
- Replace shoes with models featuring good arch support and durable soles.
- Sleep wearing special foot splints, which will stretch your injured fascia and allow them to heal.
If you suffer from an extreme case of plantar fasciitis, your doctor may prescribe more aggressive treatment options, which include:
- cortisone (steroid) injections
- wearing a boot cast for up to six weeks
- creating custom orthotics (shoe inserts) from an orthopedist
- surgery to relieve tension on the plantar fascia
The two main surgical options are to lengthen overly tight calf muscles (gastrocnemius recession), or to perform a partial cutting of the stressed plantar fascia (plantar fascia release).
However, complications of surgery include weakened arches, nerve damage, and only partial relief of the foot pain.
can Plantar Fasciitis be Prevented?
Yes. There are steps you can take to reduce your risk of developing sore fascia in your feet.
- Maintaining flexibility all through your lower legs can help prevent this condition from developing. Contact your doctor for specific flexibility exercises for your calf, Achilles tendon, and ankle.
- Gently stretch your plantar fascia each morning before getting out of bed.
- Do regular stretches for your calf and the bottoms of your feet.

- Maintain a healthy weight.
- Do not wear high heeled shoes, and do not walk barefoot, particularly on hard or uneven surfaces.
- Replace worn-out shoes in a timely manner. Runners are highly recommended to get new running shoes after every 500 miles.
- Replace high-impact sports with those that are gentler on your joints, such as bicycling, swimming, and low-impact aerobics.
This condition can be prevented and treated. The first step to relieving your pain is getting a diagnosis. If you live near Corpus Christi, Texas, call Coastal Orthopedics at 361.994.1166 to make an appointment for an examination.
Dr. Williams has been practicing orthopedic surgery in Corpus Christi since 1998. After graduating from Texas Tech hereceived his medical degree from the University of Texas at San Antonio. At the prestigious Campbell Clinic located at the University of Tennessee, Dr. Williams completed not only an Orthopedic Surgery Residency, but an additional year of Fellowship Training in Spine Surgery. Dr. Williams is dedicated to creating an excellent patient experience in the office or in the surgery suite.
Topics:

